
|

|

|

|
|
This article may be reprinted free of charge provided 1) that there is clear attribution to the Orthomolecular Medicine News Service, and 2) that both the OMNS free subscription link http://orthomolecular.org/subscribe.html and also the OMNS archive link http://orthomolecular.org/resources/omns/index.shtml are included. FOR IMMEDIATE RELEASE
Vaccines - Reassessing Their Relevance
by Greg BeattieIntroductionThe USA's incoming health administration has vowed to increase safety testing of vaccines-a move welcomed by many. However, this approach addresses only one half of the benefits/risks framework in which vaccines are judged. In this paper, I appeal for revision of the exalted place that vaccines have enjoyed in history due to their perceived benefits. It is hoped that any new risk profiles that emerge from this new direction may therefore be considered within a more nuanced framework. The role of vaccination in the dramatic declines of mortality and morbidity from certain infectious diseases has earned it an enormous reputation. This perceived relevance as the agent of change in the public health landscape is rarely questioned - and they continue to be our most hopeful solution when new threats arise. [1] Thus, from the outset, concerns about risks have typically faced fierce scrutiny-even opposition. That is the opposite of the precautionary principle. Even where adverse outcomes have been conceded, the sacrifice of a small number is said to be necessary for the greater good. Some key assumptions underpinning this perception are briefly reviewed here:
Readers are hereby invited to reconsider these assumptions in the hope that this may foster a more open and free discussion of safety concerns when they arise. Historical decline in infectious disease mortalityAlthough the dramatic reduction in infectious disease mortality over the past two centuries is frequently attributed to vaccination, examination of the data demands revision of this. [2,3] In Australia, empirical evidence [4] illustrates major declines in specific disease mortality preceding widespread vaccination for each disease. Measles deaths per capita fell by 99.5% in the century before the first measles vaccine was introduced (see Fig 1). Similarly, pertussis deaths declined 96% before mass implementation of the pertussis vaccine (DTP), and 86% before an earlier single vaccine was in limited use. Diphtheria mortality dropped 98% before DTP licensing and 85% before any use of a diphtheria vaccine. 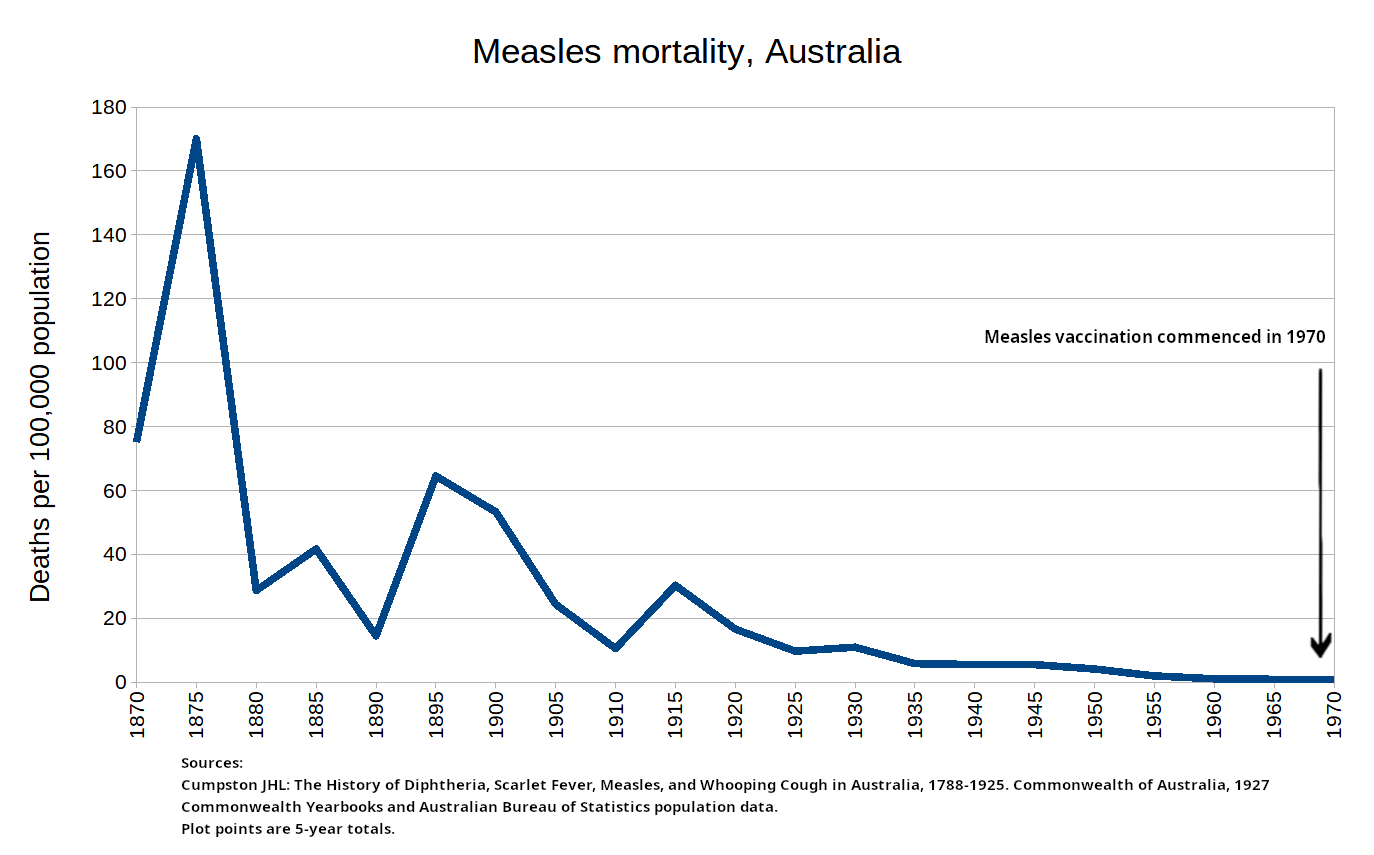
Figure 1. It must be stressed that these numbers, along with the depiction in Figure 1, make no attempt to quantify the role that vaccines may have played in any subsequent declines. They merely highlight the declines that preceded vaccines. This pattern was not unique to Australia - all countries with reliable registration systems documented similar trends. Numerous charts confirming this are available on the internet. [5] Vaccines simply did not exist when the bulk of the declines took place. We are therefore on safe grounds to conclude, without attempting to quantify their eventual input, that their historical contribution was small at best. We are equally safe in concluding that other factors were largely responsible for the total declines, and that their contributions in fact dwarfed those of vaccination. Along with more rational healthcare practices, those factors are universally acknowledged to be improvements in nutrition and sanitation. These not only preceded the vaccination effort but likely continued during it. Of these, improvements in nutrition is considered the most influential. [2] An exception to the pattern of late arrival of vaccination is of course smallpox - the smallpox vaccine was developed in 1798. Although official records indicate negligible mortality from smallpox in Australia despite very low vaccination levels, [6] other countries experienced significant mortality, and substantial declines occurred during use of the vaccine. It must be noted however that parallel declines occurred in other infectious diseases with no vaccine during the same period - clearly suggesting that improvements in other factors such as nutrition and sanitation were responsible. Figure 2 illustrates the declines in England and Wales of both smallpox and scarlet fever. [7] 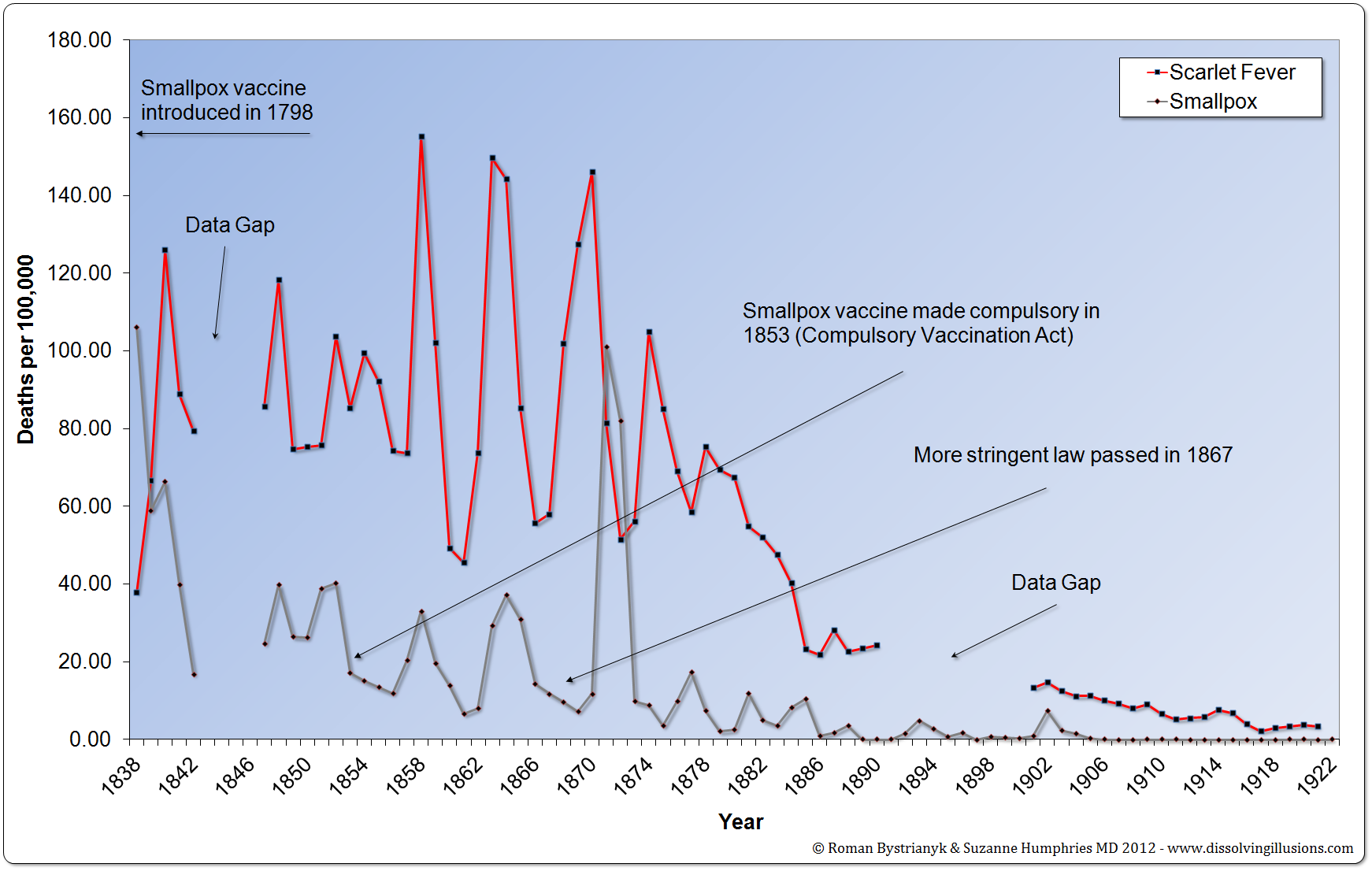
Figure 2: England and Wales smallpox and scarlet fever mortality rates from 1838 to 1922. (Record of mortality in England and Wales for 95 years as provided by the Office of National Statistics, published 1997; Report to The Honourable Sir George Cornewall Lewis, Bart, MP, Her Majesty’s Principal Secretary of State for the Home Department, June 30, 1860, pp. a4, 205; Written answer by Lord E. Percy to Parliamentary question addressed by Mr. March, MP, to the Minister to Health on July 16, 1923; Essay on Vaccination by Charles T. Pearce, MD, Member of the Royal College of Surgeons of England) Mortality benefitVaccination programs may only marginally help to lower mortality. What would happen without them? The case of Sweden provides an interesting natural experiment. [8] In 1979, Sweden removed the pertussis vaccine from its schedule, keeping it off for 17 years until 1996. Contrary to what might be expected, mortality data shows pertussis deaths [9] during the non-vaccination period (7 deaths) were no higher than either the preceding (10 deaths) or subsequent (9 deaths) 17-year periods. Conventional wisdom would suggest that the pause should have been marked by a substantial spike in deaths, but this was not the case. Figure 3 depicts the decline in pertussis deaths pre-vaccine, as well as the persistent low levels thereafter despite the removal and reintroduction of the vaccine. This is perhaps the only example of a country vaccinating, pausing for a considerable period, then resuming, with other factors remaining presumably constant. It may therefore be considered a challenge→de-challenge→re-challenge: a protocol considered very strong evidence regarding the notion of causation when observed at the population level. 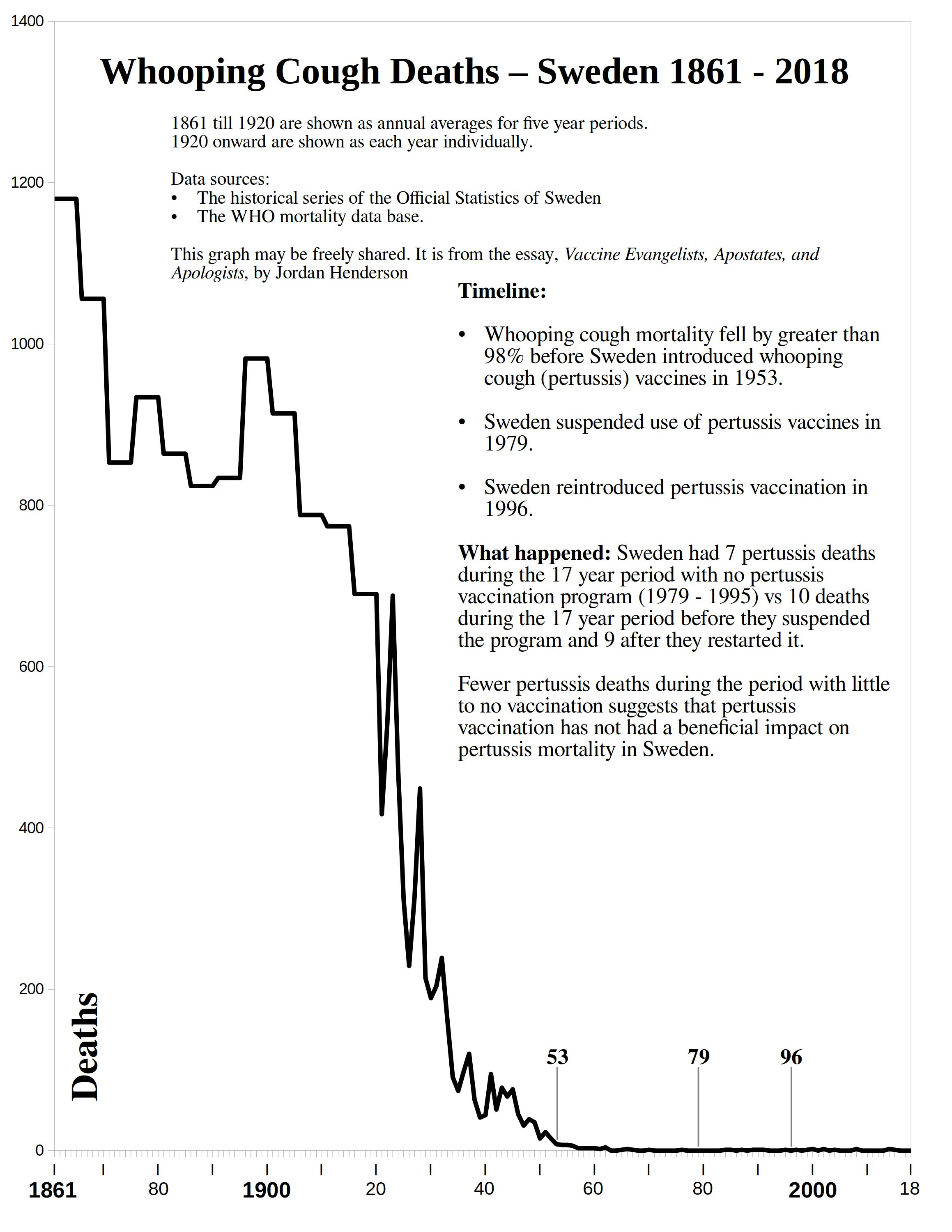
Figure 3. Also contrary to expectation, research has identified a statistically significant positive association between the number of vaccine doses routinely administered by a country and that country's neonatal, infant and under-5 mortality rates. [10] Again, conventional wisdom would lead us to predict the opposite. Claims from studies in developing countries appear to balance these examples, however those claims also require careful examination. While dramatic reductions in measles deaths have been reported by these studies and attributed to vaccination programs, [11,12] the reported reductions were not based on death counts. The majority of estimated measles deaths occur in countries that do not have adequate death registration. For these countries, estimated deaths typically derive from models that assume vaccine effectiveness. [13] The population size, the number of vaccines delivered, and the presumed level of protection they offer are the primary inputs to the model. Obviously, using the results from such a model to demonstrate the assumption on which the model is built is circular reasoning. MorbidityWhile mortality data suffer known limitations, evaluating relevance of vaccination beyond mortality presents even greater methodological challenges. Morbidity data, while important, are, by necessity, sample data and therefore rely on careful design and rigorous adherence to meaningful quantification. Disease notifications from surveillance systems, often used as a proxy, can be influenced by various factors unrelated to actual disease incidence. Major surges in disease notifications have been later determined to be artefacts of such systems. [14] In the Swedish example mentioned previously, pertussis notifications were high during the pause in vaccination (mean 8545 per year during 1979-1995). [15] Then, after vaccination resumed, they plummeted for the subsequent 17 years to roughly one-sixth (mean 1490 per year) that number. Deaths however did not decrease. These observations are difficult to reconcile. Conventional thinking predicts deaths should have soared during the pause and then retreated roughly 6-fold after resumption. If both sets of data are to be trusted, resuming vaccination led to a dramatic decrease in disease and at the same time a dramatic increase in case-fatality ratio. A more likely explanation is that notification data are not an accurate gauge of morbidity. One needs only to briefly peruse measles data from the past 30 years in the UK for an example of the lack of correlation between cases and deaths. [3] Polio morbidity data illustrates a further complexity. While reported cases of polio declined dramatically in all developed countries after vaccine introduction, diagnostic and reporting protocols changed so fundamentally that pre- and post-vaccine case numbers cannot be meaningfully compared. Modern polio diagnosis requires expert committee approval and poliovirus laboratory confirmation, whereas pre-vaccine cases were typically reported by individual practitioners based on clinical judgement alone, and these included many non-paralytic cases. [16] Randomized controlled trials (RCTs)Randomized controlled trials might seem to offer clarity, but they also present concerns. Ethical considerations typically preclude using true placebos in vaccine studies. Most modern trials are equivalence or non-inferiority-they compare new vaccines to existing ones rather than to unvaccinated controls. This means they rely on the established efficacy of their predecessors. But those predecessors typically have not undergone controlled trials, or, where they did, such trials have often used other, unrelated vaccines (sometimes experimental), [17] or vaccine solvent (including formaldehyde, thiomersal, and aluminium phosphate), [18] as placebo. Also, randomized controlled trials rarely use clinical outcomes as their primary endpoints. Instead, most measure immunogenicity. Where clinical outcomes are measured they are typically restricted to antigen-specific clinical outcomes (e.g. Hib-associated meningitis, rather than meningitis). If they are to address scepticism, randomized controlled trials need to use inert placebos and demonstrate success in lowering clinical entities using the broadest scope possible, including overall mortality. I am not aware of any controlled trial that uses an inert placebo and establishes the clear clinical value of a vaccine in routine use. Although inert placebos in vaccine RCTs have been considered unethical, a vaccine trial could include a regimen of essential nutritional supplements provided at several different doses. Because nutrition is known to be one of the major factors in enhancement of immunity essential for prevention and treatment of viral disease [3] - this could provide a way to include a truly randomized placebo while also testing for dose efficacy. [19] Candidate equivalence supplements could include combinations of vitamins A, B, C, D, with magnesium, zinc, and selenium, at multiple doses higher than the RDA. DiscussionThese historical and methodological considerations should inform current debates on vaccine policy. For benefits to be weighed against risks, benefits must be clearly understood and quantifiable without resort to questionable assumptions. Given that some vaccines are exempt from manufacturer liability in certain jurisdictions, and considering both known and potential risks, many medical professionals and community members advocate for:
The goal explored here is not to dismiss vaccines as a public health tool but to encourage re-examination of some of the assumptions which have long underpinned their use, and promote a more realistic, evidence-based evaluation of their benefits and limitations within the broader context of public health improvements. References1. Mayer Y, Etgar S, Shiffman N, et al (2021) Hope as a predictor for COVID-19 vaccine uptake. Hum Vaccin Immunother. 17:4941-4945. https://pubmed.ncbi.nlm.nih.gov/34714728 2. McKinlay JB, McKinlay SM (1977) The questionable contribution of medical measures to the decline of mortality in the United States in the twentieth century. Milbank Mem Fund Q Health Soc. 55:405-428. https://pubmed.ncbi.nlm.nih.gov/413067 3. Holford, P (2020) Did Vaccinations or Vitamins Stop Measles Deaths? Holford Health Club, 2020 Sept 30. https://www.patrickholford.com/did-vaccinations-vitamins-stop-measles-deaths 4. Cumpston JHL (1927) The History of Diphtheria, Scarlet Fever, Measles, and Whooping Cough in Australia, 1788-1925. Commonwealth of Australia. Department of Health. Service Publication No. 37. https://www.cabidigitallibrary.org/doi/full/10.5555/19292700933, https://vaccinationdilemma.com/chapters/CompanionData.zip 5. The following websites offer multiple charts: https://jordanhenderson.substack.com/p/gallery-of-graphs https://vaccinationdilemma.com/historical-death-rates-diseases-vaccination-html https://dissolvingillusions.com/graphs-images 6. Cumpston JHL (1914) The History of Smallpox in Australia, 1788-1908. Commonwealth of Australia. https://archive.org/details/39002011127157.med.yale.edu/mode/2up?view=theater 7. Humphries S, Bystrianyk R. Dissolving Illusions. Available from https://dissolvingillusions.com/graphs-images 8. Henderson J. (2023) Vaccine Evangelists, Apostates, and Apologists: Part 5. https://jordanhenderson.substack.com/p/vaccine-evangelists-apostates-and-7f5 9. WHO Mortality Database. Available from https://platform.who.int/mortality/themes/theme-details/topics/indicator-groups/indicators/indicator-details/MDB/pertussis 10. Miller NZ, Goldman GS (2023) Neonatal, Infant, and Under Age Five Vaccine Doses Routinely Given in Developed Nations and Their Association With Mortality Rates. Cureus 15: e42194. https://pubmed.ncbi.nlm.nih.gov/37484788 11. WHO (2007) Measles deaths in Africa plunge by 91%. https://www.who.int/news/item/28-11-2007-measles-deaths-in-africa-plunge-by-91 12. Wolfson LJ, Strebel PM, Gacic-Dobo M, et al., Measles Initiative (2007) Has the 2005 measles mortality reduction goal been achieved? A natural history modelling study. Lancet. 369:191-200. https://pubmed.ncbi.nlm.nih.gov/17240285 13. Kenji Shibuya (2007) Decide monitoring strategies before setting targets; Bulletin of the World Health Organization, June 2007, 85:423. https://www.scielosp.org/article/bwho/2007.v85n6/423-423/en 14. Scheil W, Cameron S, Roberts C, Hall R (1998) Pertussis in South Australia 1893 to 1996; Comm Dis Intel. 22:76-80. https://www1.health.gov.au/internet/main/publishing.nsf/Content/cda-pubs-cdi-1998-cdi2205-cdi2205c.htm 15. World Health Organization (WHO) (2023) WHO Global Health Observatory Pertussis Reported Cases by Country 1974-2022. Geneva, Switzerland: World Health Organization (WHO). https://ghdx.healthdata.org/record/who-global-health-observatory-pertussis-reported-cases-country-1974-2022 16. Nathanson N, Martin J (1979) The epidemiology of poliomyelitis: enigmas surrounding its appearance, epidemicity, and disappearance. Am J Epid: 110:672-692. http://aje.oxfordjournals.org/content/110/6/672.full.pdf+html 17. Prevention of Whooping-cough by Vaccination. Medical Research Council Investigation. Br Med J. 1951 Jun 30;1:1463-1471. https://pubmed.ncbi.nlm.nih.gov/14839295 18. Ad Hoc Group For The Study Of Pertussis Vaccines (1988) Placebo-controlled Trial of Two Acellular Pertussis Vaccines in Sweden; Protective Efficacy and Adverse Events. Lancet, 331:P955-P960. https://doi.org/10.1016/S0140-6736(88)91778-3 19. Wimalawansa SJ (2025) Vitamin D Deficiency Meets Hill's Criteria for Causation in SARS-CoV-2 Susceptibility, Complications, and Mortality: A Systematic Review. Nutrients, 17:599. https://pubmed.ncbi.nlm.nih.gov/39940457 Orthomolecular MedicineOrthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org Find a DoctorTo locate an orthomolecular physician near you: http://orthomolecular.org/resources/omns/v06n09.shtml The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource. Editorial Review Board:
Jennifer L. Aliano, M.S., L.Ac., C.C.N. (USA)
Comments and media contact: editor@orthomolecular.org OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication. To Subscribe at no charge: http://www.orthomolecular.org/subscribe.html To Unsubscribe from this list: http://www.orthomolecular.org/unsubscribe.html |

This website is managed by Riordan Clinic
A Non-profit 501(c)(3) Medical, Research and Educational Organization
3100 North Hillside Avenue, Wichita, KS 67219 USA
Phone: 316-682-3100; Fax: 316-682-5054
© (Riordan Clinic) 2004 - 2024c
Information on Orthomolecular.org is provided for educational purposes only. It is not intended as medical advice.
Consult your orthomolecular health care professional for individual guidance on specific health problems.