 |

|
 |

|
 Back to 1996 4th Quarter Table of Contents
Back to 1996 4th Quarter Table of Contents
Introduction Cholesterol (Figure 1) is a deadly poison which we must avoid at all costs. That is the fad which is being pounded into us by unthinking doctors and popular magazines. How true is it? Perhaps it has the appearance of truth because of the following facts:
The BeginningsI am an amateur astronomer. I am interested, among many other aspects of astronomy, in what the radio astronomers are finding out about the chemistry of the clouds of gas and dust out of which stars and planets form. All kinds of complex chemicalshavebeenfoundinsuchclouds.1 Cholesterol has not been found. That is because the radioastronomers donot know its radio signature. They do not know how to find it. I have shown elsewhere that it is a reasonable, but not as yet provable, assumption that, when the Earth formed about four and a half billion years ago, cholesterol was already present.2 The evidence appears to indicate that life appeared upon the Earth within a hundred million years of its formation–an astonishingly short time. And cholesterol was involved in life right from the very start. Around every living thing is a membrane,envelope, which governs the movement of chemicals in and out of the organism. Cholesterol is one of the main elements holding the membrane together. Somewhere between six hundred and eight hundred million years ago there was a great revolution in life, the rise of eukaryotic (with a nucleus and other special is edinternal mechanisms)cellsfromthe prokaryotic (without a nucleus and other complex mechanisms) cells. It seems to have happened by different cells/organism forming associations for their mutual advantage. For example, the mitochondria, or “power plants” inside our cells have been shown to be semi-independent cells in their own right with their own reproductive/hereditary machinery.This revolution led to the change of the atmosphere from one without free oxygen to one with this important gas, and to the evolution of the higher organisms like ourselves. All these internal mechanisms are membrane based and depend upon cholesterol for their functioning and integrity. Amongst the higher animals there are such strange divisions a smal esand females. It is the genes (the hereditary material with in the nucleio four cells)which decide which is which,but the genes do it through the sex hormones. The sex hormones, and some others too,are all manufactured from cholesterol. For these reasons cholesterol seems to be not the poison that some people want us to believe, but one of the most vital substances to life. So why is there this fuss over cholesterol? HO 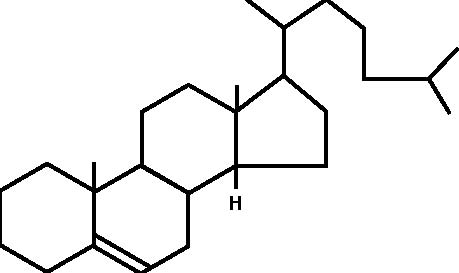 Figure 1. The Molecular Structure of Cholesterol The FussThe simplistic, naive picture that is being pushed on, and by, the medical profession as a whole is that this sticky stuff, cholesterol, drifts along in the blood stream. If, and only if, there is damage to the blood vessel–a very important point –then the sticky cholesterol attaches itself to the wall and builds up there in the form of the plaques which I mentioned above. There is no mention of the fact that cholesterol has no role in the early development of the plaques which actually form when smooth muscle cells from the middle layer of hewalloftheartery,the media ,migrate into the interior, the lumen. It is the seabnormally sited cells which form the basis of the plaques to which the cholesterol and, it must be re-emphasized, other substances stick (Figure 2). Only after the plaque has formed is there any deposition of cholesterol, and other substances, in the plaque. The stickiness of cholesterol is entirely irrelevant. Why measuring cholesterol alone is not enough is that there is an undoubted protective mechanism also in the blood. This is called High Density Lipoprotein (HDL) and consists of small protein molecules which pry the stuck cholesterol back out of the plaques and remove it safely for destruction by the liver. By far the better way of measuring the risk of having a heart attack or stroke is to divide the cholesterol by the HDL. If the resulting number is 4.4, or less, there is a relatively low statistical risk of having a heart attack or stroke. If the number is higher than 4.4., then there is an increased statistical risk of these conditions. Remember, these are statistical risks, not certainties, i.e. a low risk factor is no guarantee that you will avoid a heart attack or stroke, nor is a high risk factor a guarantee that you will experience such illnesses. For example, my plump, smoking grandmother died aged nearly 102 years old. So the obvious conclusion is either we ought to lower the levels of cholesterol, or raise the HDL, or both. As an aside, another factor frequently measured is Low Density Lipoprotein (LDL). The evidence of a direct role of LDL in atherogenesis is shakey. There is better evidence that oxidised LDL is important. In British Columbia we are not allowed to measure oxidised LDL. So how do we lower the levels of cholesterol? Since cholesterol occurs variably in the diet and we can measure how much of it appears in the blood, then it seems logical to lower the amount of cholesterol in our diets. What is wrong with that? Dietary CholesterolSeveral things are wrong with the idea of lowering cholesterol by diet: 1. It has been known for more than a quarter of a century, and was taught to my class in medical school by the revered Professor of Pathology, Tom Symington, at the Royal Infirmary in Glasgow, that if we label cholesterol with a radioactive Cholesterol, a Personal Viewpoint isotope and feed it to volunteers, none of it becomes attached to the blood vessel walls in the plaques. None of it! 2.Anyway,the maxim umamount that we can lower cholesterol by reducing it in our diets is 9% (granted that, in the rare case, it can be as much as 18%), which is trivial. 3.Mostimportantly, what is the actual result of lowering the amount of cholesterol in the diet? The Finns have been doing this on a large scale for longer than anyone else. What are their results? a) Over the first five years there is a lowering of the death rate due to heart attacks and strokes–to the extent of 20 days, that is less than three weeks! But the total death rate goes up! How? There is an excess number of deaths due to suicide, accidents and violent deaths. Why is unknown. My personal, unconfirmable belief is that life on a low cholesterol diet is so miserable that the patients’ behaviour becomes disturbed. b) Between five and ten years, the benefits as far as heart attacks and strokes disappears. But the excess of other deaths remains. c) Beyond ten years the death rate of heart attacks and strokes is higher! And the excess of other causes of death still remains. So trying to lower the death rate from heart attacks and strokes by lowering the amount of cholesterol in the diet is quite futile. The Other Risk FactorsThere are more important risk factors for heart attacks which have nothing to do with cholesterol. Firstofall,thereisnopointinworrying aboutcholesterolinsomeonewhorefusesto stop smoking. Smoking is by far the greater lifestyleriskasfarasheartattacksandstrokes is concerned. And it causes death through so many other diseases as well. Secondly, there is also little point in worrying about cholesterol in someone who has high blood pressure which is not being controlled. Uncontrolled hypertension is, like smoking, a much greater Figure 2. Cross Section of an Artery Showing the Start of Atheromatous Plaque (Hardening of the Arteries) with no Cholesterol Involvement 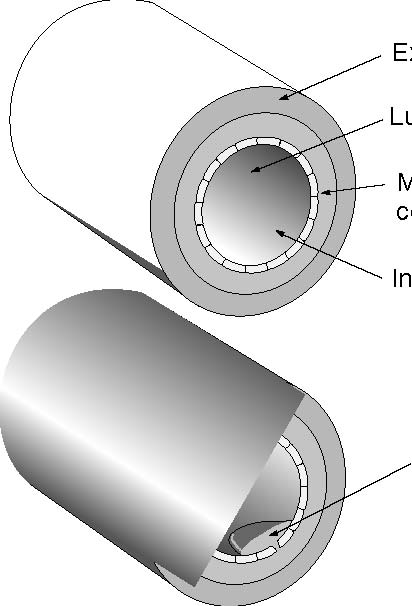 Externa, the support structure Lumen, where the blood Media, the smooth muscle cells which control the tone of the artery wall Intima, the cells lining the artery Medial cells migrating through the intima into the lumen Figure 3. The Detailed Route by which Cholesterol is Manufactured (especially important factors are shown in bold type) Glucose Fructose-6-phosphate� and Fructose as fruit sugar, is entered into the pathway here 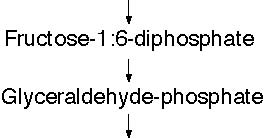 1:3 -diphospho-Glycerate 3-phosphos-glycerate 2-phosphos-glycerate Phospho-enolpyruvate Acetyl-Coenzyme A� a very important molecule, the starting point of many other reactions HMG CoA � (b-hydroxy-b-methyl-glutaryl-Coenzyme A) Mevalonate 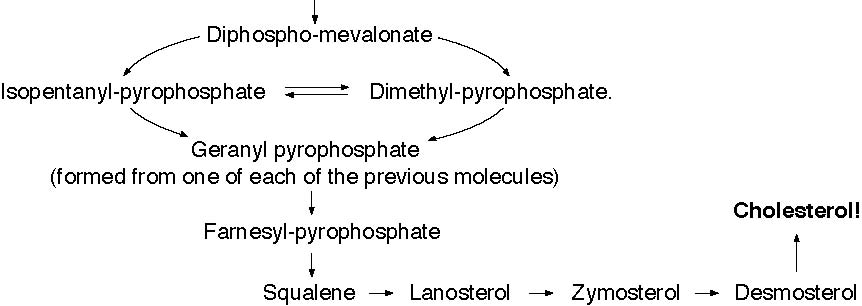 risk for heart attacks and strokes. But we cause heart attacks and strokes. have to make sure that a person is truly Thirdly, if a patient has diabetes, hypertensive before we embark on measwhether the blood sugars are controlled ures which lower the blood pressure. To or not, the blood vessel changes leading to treat someone for hypertension who is not heart attacks and strokes proceed rapidly hypertensive is very dangerous, and, by unless quite a different approach is also bringing the blood pressure too low, can Cholesterol, a Personal Viewpoint used (see about vitamins below). Admittedly cholesterol is involved here, but its precise role is not clear at all. Equally, oxidised LDL is also involved. Fourthly, the combination of uncontrolled hypertension and diabetes is particularly lethal. Even worse is the combination of smoking, uncontrolled hypertension and diabetes. Fifthly,what is the actual source of the cholesterol which does attach to the blood vessel wall? The SourceIf it is not dietary cholesterol, where does it come from? The pathway by which cholesterol is formed in the body occurs in the liver and starts with a chemical called Acetyl Coenzyme-A (acetyl Co-A), a very important substance in so much of body chemistry (see Figure 3). By far the most acetyl Co-A comes from glucose and fructose, both of which are constituents of white sugar and starch. It has been known for along time that populations with diets low in refined foods, meaning low in sugars and simple starches, have a low incidence of heart attacks and strokes.3 Indeed it is virtually unknown to them–unless they start eating the so-called “civilized diet” with its adulteration by sugar and simple starches, along with artificial flavourings, colourings and preservatives.Conversely,in populations with diets high in refined foods heart attacks and strokes are very common. Another line of evidence is very important. The great age of Pathology was the 19th century. The signs of myocardial infarction (MI) are very clear, but were never described by the great pathologists in any of their autopsies. They could not have missed them! It was only when white flour and sugar became cheap and widely available in this century that the signs of MI began to be described. AdviceOne: If you want to follow a diet which prevents heart attacks and strokes, avoid refined foods. There are other benefits. Also the Mayo Clinic carried out a study comparing what happens to us if we eat the usually recommended three square meals per day, or if, after a good breakfast, we have small,frequent snacks throughout the rest of the day, avoiding being hungry. Amongsttheotherbenefitsofthisisalowering of the cholesterol levels and a raising of the HDL levels. This advice has been confirmed by many other studies. 4-13 Advice Two: Have a good breakfast every day, and then no other big meals, but frequent,small snacks.Incidentally, do not bother about a low fat diet, unless you have raised fat (triglyceride) levels in your blood.Its effect is negligible on cholesterol. And the people with the very highest fat diets, the Inuit and Masai (provided they are eating their normal diet,not ours)have no incidence of heart attacks and strokes at all.14 What about other ways of lowering cholesterol? Do they do any good? Do they allow people to live longer? Do Drugs Help?Many drugs are on the market whose effect is to lower cholesterol. Most of them are directed at blocking the conversion b-hydroxy-b-methyl-glutaryl-Coenzyme A to Mevaldate. (see Figure 3), the so-called HMG CoA Reductase inhibitors, the “Statins.” Some of them also raise HDL. Until recently the research that alleges that they do prolong life has been shown to be systematically fudged, although not deliberately so.15 Recently there has been considerable publicity about claims that they might reduce MI by 35%, which is a startling claim. The reality is more sobering and is worth looking at carefully. In the 4S16 study 123 patients would have to be treated for one year at a totalcost of either $51,600 Canadian or $103,200, depending on the dose of simvastatin used, to prevent one death from MI. Twenty-five patients would have to be treated for five years for one death to be prevented, at a total cost of $107,500 or $215,000. In the WofS17 study 700 patients would have to be treated for one year at a totalcostof$996,100topreventonedeath from MI. A similar cost would have to be incurred over five years for 140 patients for one death to be prevented. Both studies were carried out over a maximum period of five years–a most important consideration when alternatives, niacin in particular, are taken into consideration. Is this cost effective? In isolation it may seem to be, but at best it is very marginal.18,19 The questions that patients are going to have to ask themselves are: 1.Whose life is it anyway that is going to be saved? Is it mine? Or am I going to have to take this drug for many years without knowing at all that it is going to do me any good? (Remembering that the reason for lowering the cholesterol is to prevent an MI, since a high cholesterol as such is without symptoms).
NiacinOne substance alone, which lowers cholesterol, raises HDL and lowers circulating fats (another risk factor), has been shown to prolong lives over more than fifteen years–even remaining effective for years after people have stopped taking it. This is niacin (nicotinic acid–a form of vitamin B3, Figure 4). In doses of three thousand to six thousand, or more, milligrams per day it is effective.20 In lesser doses no effect has been shown. No effect either is detectable with the other forms of vitamin B3, such as niacinamide. There are minor difficulties with niacin:
It causes the famous niacin flush. 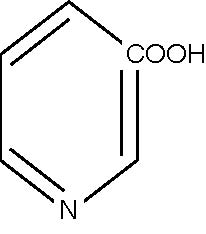 Figure 4. The Chemical Structure of Niacin tion. This is due to the same mechanism as the niacin flush, but affecting the acid producing cells of the stomach. But there is some evidence that, over prolonged periods, it may heal ulcers.
Specifically, there is no recorded case of any patient taking Niacin who has gone into liver failure. On the other hand other drugs prescribed to lower cholesterol are prone to causing liver damage. Niacin has other beneficial effects, including lowering blood pressure, counteracting some of the harmful effects of nicotine, improving the general circulation, acting as a mild tranquillizer (without the bad effects of tranquillizers), and increasing the survival rate of patients with cholera. Advice Three: Start taking niacin–but only under medical supervision. I recommend starting niacing by the following means to mitigate the niacin flush, but if the patient is willing he/she may jump to the full three gram dose per day: Start with 100mg tablets. Take 1/2 three times per day after meals for one week. Then take 1 three times per day after meals. Switch to the 500mg tablets. Take 1/2 three times per day after meals for one week. Then take 1 three times per day after meals for one week. Then take 2 three times per day after meals for the rest of your life. The reason for starting the niacin like this is the famous niacin flush. In the body throughout the reare cells called mast cells. These contain stores of chemicals/ hormones, such as histamine and bradykinin. The niacin causes the mast cells to release these substances which are the cause of the niacin flush, not the niacin itself. But the stores take time to build up again. So the more niacin you take the more you exhaust the stores and the quicker you become free of the flush. On the other hand, if you forget to take even one dose, the stores are able to build up again and you are back to square one. The same mechanism causes indigestion in some people early on taking niacin, but this soon stops. Another advantage for women who are postmenopausal is that the niacin causes their fat cells to produce more sex hormone and this helps to prevent osteoporosis. There is no evidence that the flush, however uncomfortable it may be, does any harm. The Real VillainBut we still have a major problem. Cholesterol, a Personal Viewpoint Heart attacks and strokes insist on happening in non-smokers,with normal blood pressures, normal blood sugars and with normal cholesterol and HDL levels who consume a diet free of refined foods. The issue we have not dealt with is –how does the cholesterol attach itself to the blood vessel wall? This is important because, sticky or not, free cholesterol in the blood does not stick to the blood vessel wall. This is where the most up to date research has shown us the way to understand the problem of cholesterol better than ever before. Lipoprotein (a), (Lp(a)), is a complex chemical (Figure 5) consisting of a large globule of cholesterol and phospholipids surrounded by a binding protein molecule (Apolipoprotein B-100) to which, in turn, is attached Apolipoprotein(a). It is this last which is responsible for cholesterol to be carried to, and bound to, the blood vessel wall. There is no evidence that cholesterol gets there by any other means in any significant amount. A lot of research has shown that Lp(a) is an adaptation of another very important substance,plasminogena dissolver of blood clots, which is vital to life,21 and is a combination of the same protease as in Lp(a) 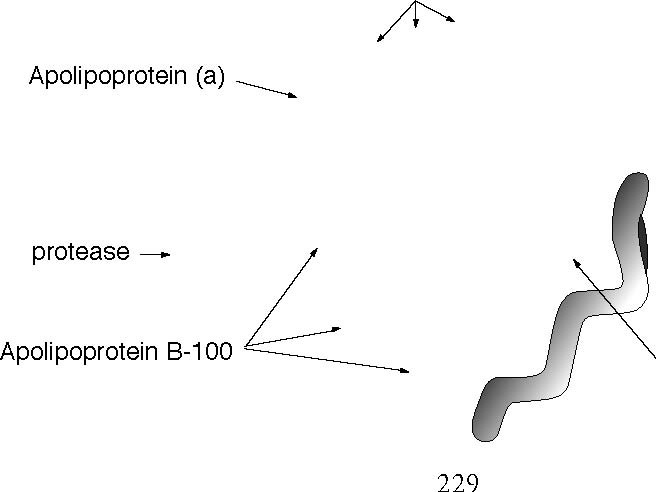 Figure 5. A Diagrammatic Representation of Lipoprotein (a) kringle groups Globule of cholesterol and phospholipid and a shorter version of the Kringle chain. Lp(a), among many other activities, seems to inhib it the action of plasminogen,which is another way in which it can promote heart attacks and strokes. Why should we have such a suicidal substance in us? The answer is that it was not designed to be suicidal but actually life saving. The Other SubstancesLinus Pauling, the greatest chemist of this century and the only man in history to have won two Nobel Prizes by himself, carried out, with many other colleagues, a great deal of research into vitamin C, or ascorbate (Figure 6). Recently attention has been turned to how vitamin C relates to Lp(a).22 About thirty to forty million years ago, a mutation occurred in our direct ancestors. Because of this the anthropoid apes, humans included, could no longer manufacture their own vitamin C. It may be that this led us to develop intelligence as a means to make our search for vitamin C containing foods more effective–an interesting, but unprovable speculation.23 ThemainroleofvitaminCistorepair damaged blood vessels. The first sign of a deficiency of the vitamin is bleeding, such as gums, or bruising. If it persists we bleed to death. Nature does not like to leave any species without protection of some sort. So Lp(a) was developed as a back up repair mechanism for damaged blood vessels. The globule of cholesterol is delivered by Lp(a) to the site of damage to plug the hole, so to speak. But, like all back up mechanisms, it is not as good as the real thing. It does not know when to stop once it starts being used. It treats sites where it has already deposited cholesterol as damaged sites to be plugged more, leading to the build up into theplaques.Thatisnotaproblemwhenwe are young. But it begins to be a problem when we pass the age of thirty five. We are HHH HOC C H OH 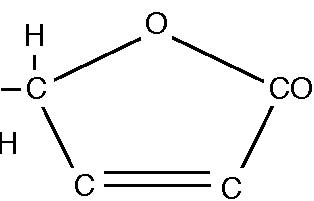 OH OH Figure 6. The Chemical Structure of Ascorbic Acid not designed to live much beyond the age of thirty five to forty. Throughout most of history someone older than thirty five was “old.” And it is when we pass the age of thirty five that the plaques really begin to be a problem. But the Lp(a) is a back up mechanism tovitaminC,not being needed when there are ample amounts of the vitamin to carry out blood vessel plumbing by itself. So we would expecta relationship between them. And there is! When the Lp(a) is measured in a patient and vitamin C is given in optimum doses,the Lp(a)declines.24 Moreover, there are increasing numbers of medical studies, the first being as far back as 1977, which show that large doses of vitamin C do prevent heart attacks and strokes, reported by a Dr. Spittals. Her career was nearly ruined because she dared to make such claims then! Can taking such large doses cause any harm at all? There is not the slightest evidence that this is so despite the best effort of medical “authorities” to find such evidence. The first sign that too much vitamin C is being taken is the development of looseness of the bowels.25 But this is the best way of finding what dose is the bestfor the person–to take it three or fourtimes per day in increasing doses until bowel tolerance is reached. Then the dose is cut to the largest dose at which stool loosening does not take place–ideally two bowel movements per day, no thicker than the little finger, of the consistency of soft toothpaste, and comfortably easy to pass. In fact the bowel tolerance is a good measure of the health of a person. If the looseness comes back, forcing a lowering of the dose of the vitamin C, invariably this goes along with an improved sense of well-being and an improvement of the general health of the patient. Conversely an increase in the bowel tolerance means a deterioration of the health of the patient. Vitamin C has many other benefits, such as helping to protect blood vessels against the damaging effects of diabetes, whether the diabetes is well controlled or not. This technique is the same whatever problem is being tackled with this agent. Advice Four: Take the optimum dose of vitamin C. Other vitamins are being tested for effect. Vitamins E and A seem to have a similar value to vitamin C. It is believed that they work through their antioxidant effect–a rather complex idea. I happen not to believe that this is the reason for their effectiveness, but that is another story. They, also, are important in the protection against the harmful blood vessel effects of diabetes. AdviceFive: Take at least four hundred units of vitamin E per day, and either a cod or a halibut liver oil capsule per day, or more under medical advice. ResultsThe above approach has worked with everyone who has tried it. I recheck at intervals of sixm onths until the desirable levels are reached and then combine rechecks with the annual physical examinations. I acknowledge that this approach is not susceptible to the usual method of placebo controlled clinical trial because there are five variables being used not one. But this is a summation of a wide variety of research from many different sources, orthodox and unorthodox. Equally I have not accumulated what I regard as enough statistics for meaningful conclusions about the long term effectiveness. No one using this approach has died, yet. But I admit that I have been using it in this form for only about four years. As further results emerge, in about another ten years, I shall report further progress. References
144. 10.Idem, Metabolic effects of meal frequency on normal young men. J Am Dietetic Assoc, 61: 391-398, October 1972. 11.Idem: Metabolic advantages of spreading the nutrient load: effects of increased meal frequency in non-insulin-dependentdiabetes, Am J Clin Nutr, 1992; 55: 461-467. 12.Idem:Metabolic effects of reducing rate of glucose ingestion by single bolus versus continuous sipping, Diabetes, 1990: 39: 775-781 13.Cheraskin E: The breakfast/lunch/dinner ritual, J Orthomol Med, 1993; 8: 6-10. 14.Cleave TL: The Saccharine Disease, New Canaan, CT. Keats Publ Inc, 1975. 15.Ravnskov: British Med J, 7: 1992 16.Scandinavian Simvastatin Survival Study Group, Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: The Scandinavian Simvastatin Survival Study (4S), Lancet, 1994; 344: 1383-1389. 17. Sepherd J, et al: Prevention of coronary heart disease with pravastatin in men with hypercholesterolæmia (WofS), NEJM, 1995; 333: 1301-1307. 18. McCormack JP & Levine M: Meaningful interpretation of risk reduction from clinical drug trials. Annals of Pharmacol, 1993; 27: 1272-1277. 19.McCormackJP&RangnoRE:Anevaluation and critique of the use of lipid-lowering drugs in a population base of 400,000 patients over the age of 65, Can. J. Clin. Pharmacol., 1994; 1: 27-32. 20.Canner PL, et al: Fifteen year mortality in coronary drug project patients: Long-term benefit with niacin, J Am Coll Cardiol, 1986; 8: 1245-55. 21.Lawn RM: Lipoprotein(a) in heart disease, Scientific American Med, 1993; 12-18. 22.Rath M & Pauling L: A unified theory of human cardiovascular disease leading the way to the abolition of this disease as a cause for human mortality, J Orthomol Med 1992: 7: 5-15. 23.Rath M: Solution to the puzzle of human evolution. J Orthomol Med , 1992; 73-80, 7: 2.
|

This website is managed by Riordan Clinic
A Non-profit 501(c)(3) Medical, Research and Educational Organization
3100 North Hillside Avenue, Wichita, KS 67219 USA
Phone: 316-682-3100; Fax: 316-682-5054
© (Riordan Clinic) 2004 - 2024c
Information on Orthomolecular.org is provided for educational purposes only. It is not intended as medical advice.
Consult your orthomolecular health care professional for individual guidance on specific health problems.